Pneumonia Oxygen Therapy: The Effectiveness of Oxygen for Adult Patients
It does not take a medical degree to understand that pneumonia affects your oxygen levels. In the simplest terms, pneumonia will cause your lungs to become inflamed, and because of that inflammation, you cannot get enough oxygen into your bloodstream.
The most obvious outward physical sign of this lack of oxygen is bluish lips or nail beds, which will quickly indicate to a physician that you are not getting enough oxygen in your bloodstream. This could be due to pneumonia or a variety of other illnesses, from chronic obstructive pulmonary disease (COPD), to asthma, to sickle cell anemia.
Once a physician determines the patient has pneumonia, oxygen therapy may be considered as a way to treat the illness. It is by no means the only treatment option, but it can be one of the most effective. We will take a closer look at how oxygen therapy works after reviewing how and why pneumonia develops.
WHAT IS PNEUMONIA?
A common illness that affects millions of people of all ages, pneumonia is an infection that stems from three different causes:
- Viruses
- Bacteria
- Fungi
The last category is rare, though some patients develop pneumonia after exposure to contaminated soil or bird droppings. Most pneumonia cases fall into the first two categories.
Viral pneumonia is typically less severe than bacterial pneumonia, though it can still make a patient quite ill and it should always be treated promptly to avoid complications or the virus worsening. Children with pneumonia have often developed it after a bout of respiratory syncytial virus (RSV), and adults often develop pneumonia if they have influenza.
Bacterial pneumonia, on the other hand, occurs often after the flu or other viruses. The blame for this illness usually rests on a germ known as streptococcus pneumoniae. Bacterial pneumonia usually affects only one part of the lung.
PNEUMONIA SIGNS AND SYMPTOMS
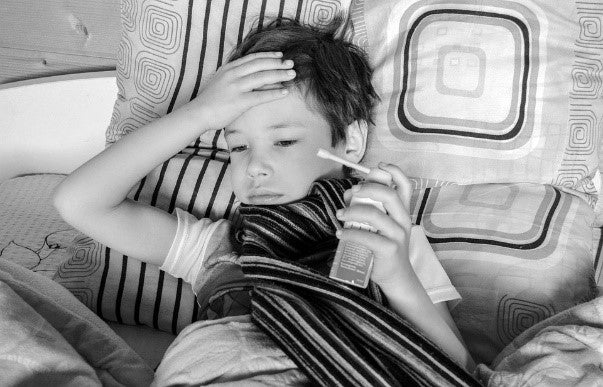
While many of us find a way to work through a common cold, seasonal allergies, or a mild stomach bug, pneumonia will typically send patients straight to bed.
Extreme fatigue can be one of the worst symptoms, and in some cases, can linger for weeks or even months. Along with fatigue, some of the first signs and symptoms a patient has developed pneumonia include:
- A cough that produces mucus
- Nausea and vomiting
- Shortness of breath
- Loss of appetite
- Fever
Additionally, the lack of oxygen reaching the bloodstream could mean patients develop confusion, which is especially common with older adults. Many individuals will describe a general achiness or muscle pain during pneumonia, along with fatigue and low energy levels.
HOW IS PNEUMONIA DIAGNOSED?
One of the trickiest things about pneumonia is that its symptoms overlap with other illnesses such as influenza. For example, patients complaining of a cough and fever could have anything from strep throat to the flu to bronchitis.
Additionally, certain age groups may differ in their symptoms for example, sometimes children with pneumonia have primarily gastrointestinal symptoms.
To determine if you have pneumonia, a healthcare provider will ask many questions about symptoms and also perform a physical exam, with a focus on listening to the sounds of your chest through a stethoscope. Crackling sounds during inhalation may be one clue that a patient does in fact have pneumonia.

The physical exam may also lead to other diagnostic tests, including:
- A pulse oximetry test, which measures the level of oxygen in your blood
- A sputum test (where a sample of mucus is examined)
- A chest x-ray
- Trouble Sleeping Brought On By Coughing And Shortness Of Breath
- Blood tests
Oxygen Therapy for Pneumonia
Once a healthcare provider diagnoses pneumonia, there are a variety of ways patients are treated to reduce the severity of symptoms and shorten the duration of the illness. The truth about pneumonia is that there is no substitute for adequate rest (we will get to more on that below). This is crucial to the recovery period.
In addition to rest, other measures can be taken to ease symptoms and help patients feel better, one of which is oxygen therapy. Supplemental oxygen is often used in severe cases of pneumonia, especially with older patients. If oxygen therapy is administered in a hospital setting, the patient will also likely benefit from fluids administered from an IV (to address dehydration, which can be common with the illness) as well as antibiotics (if the pneumonia is bacterial).
Pulse oximetry tests will often be the determining factor if oxygen therapy is needed. For healthy individuals, the blood oxygen level will usually fall between 95% and 100%. Those numbers tell us your red blood cells are effectively carrying oxygen to your cells and tissues.
When the blood oxygen level registers between 90% and 92%, a patient may need supplemental oxygen, and any reading below 90% indicates immediate medical attention and intervention is required. Hypoxemia is the medical term for a low blood-oxygen level, and it should always be monitored and treated by a physician.
Oxygen therapy can also be referred to as a “breathing treatment” and this means we receive extra oxygen via nasal cannula, a face mask, or in extremely serious cases a ventilator. This would include patients in respiratory failure who would be treated in an ICU setting.
In many cases, pneumonia patients whose symptoms are not life-threatening would be candidates to receive oxygen via an oxygen concentrator, which is less expensive than a tank or cylinder. Supplemental oxygen delivers to the lungs air that is 99% pure oxygen, versus the air we normally breathe made up of about 20% oxygen.
The use of any kind of oxygen therapy or equipment should be monitored and prescribed by a physician, and patients should never change an oxygen flow rate on a device without consulting their doctor first. Professional medical oversight is critical when battling serious infection and respiratory illness. A lack of proper treatment could mean a patient ends up in severe respiratory distress.
FAQS ABOUT OXYGEN THERAPY FOR PNEUMONIA
How Much Oxygen Will I Need?
Every case of oxygen therapy will be unique to the individual: physicians and respiratory therapists will dictate the amount of oxygen appropriate for the patient based on the results of pulse oximetry and other tests.
Is Too Much Oxygen Dangerous?
Yes! Too much oxygen can actually damage the cells in your lungs, which is another reason why supplemental oxygen should always be monitored by a trained medical professional.
Can I Smoke While Using Oxygen?
The answer to this question is an emphatic NO. First and foremost, it is incredibly unsafe in that any open flame near oxygen could trigger a combustible reaction. Beyond that, smoking will only make your pneumonia symptoms worse. There is no better time to quit than now! The American Lung Association has some great resources for those interested in smoking cessation.

Is There a Specific Storage Temperature for Oxygen Devices?
Temperature is important to the successful operation of supplemental oxygen devices. If you are using an oxygen concentrator at home, be sure to refer to the specific instructions from the manufacturer. Generally, devices will need to be store in temperatures between 60 and 70 degrees Fahrenheit.
What Other Illnesses are Treated with Supplemental Oxygen?
The use of supplemental oxygen is not limited to pneumonia patients. A wide variety of illnesses and diseases call for supplemental oxygen at various stages, including chronic obstructive pulmonary disease (COPD), asthma, cystic fibrosis, pulmonary fibrosis, and sleep apnea.
Other Ways to Treat Pneumonia
While supplemental oxygen may be ordered if pneumonia becomes severe, there are several treatments and steps taken first to ease symptoms and promote recovery.

Physicians will tell patients first to rest, rest, and then rest some more. Pneumonia recovery is largely attributed to rest, which can be a challenge for those who maintain an active lifestyle. However, taking the time to let your body heal with adequate rest is the best thing you can do to recover from pneumonia.
Antibiotics are prescribed to those with bacterial pneumonia; however, they will not effectively treat viral pneumonia. In those cases, some prescription-strength antiviral medications are available.
Over-the-counter pain relievers and fever reducers can help ease symptoms, and maintaining fluids is important to prevent dehydration. A nutrient-rich, well-balanced diet is helpful when fighting illness and infection, too.
FINAL THOUGHTS ON OXYGEN THERAPY FOR PNEUMONIA
Supplemental oxygen can be helpful in those cases where pneumonia is severe enough to lead to hypoxemia. It should always be managed and monitored by a medical professional, and it may be one step in treating the patient, along with medication and adequate rest.
Oxygen therapy is a useful and effective tool when administered properly, but it does not come without significant risk if used incorrectly. Supplemental oxygen devices should always be handled and stored with great care and kept out of reach of minors. If you have any questions or concerns about supplemental oxygen or are experiencing symptoms of respiratory distress, seek medical attention right away.
Average Lung AirPhysio
ENJOY BETTER BREATHING - Use this 100% Drug Free Device - AIRPHYSIO

Recent Posts
Sports AirPhysio
IMPROVE YOUR SPORTING PERFORMANCE - Use this 100% Drug Free Device - AIRPHYSIO

AirPhysio Child
BETTER BREATHING FOR YOUR CHILD - Use this 100% Drug Free Device - AIRPHYSIO

Categories
- asthma (2)
- atelectasis (2)
- bronchiectasis (2)
- copd (3)
- cystic-fibrosis (45)
- featured (10)
- uncategorized (2)


